In today’s highly competitive market, businesses must constantly refine their pricing strategies to stay ahead. Traditional pricing methods, often reliant on historical data and manual processes, can be slow to adapt and may not fully capture the complexities of today’s dynamic market conditions. This is where Artificial Intelligence (AI) steps in and offers powerful tools to optimize pricing in real-time. By analyzing vast amounts of data, such as customer behavior, market trends, and competitor pricing, AI enables businesses to create more accurate and responsive pricing models that maximize both profitability and market competitiveness.
AI-driven pricing analytics provide businesses with the ability to dynamically adjust prices, ensuring they remain agile in a constantly shifting landscape. Through advanced algorithms and machine learning, companies can not only predict demand fluctuations but also tailor their pricing strategies to individual customer segments, improving both revenue and customer satisfaction. In this blog, we’ll explore how AI-powered solutions are revolutionizing pricing strategies, providing companies with the insights needed to make smarter, data-backed decisions that lead to optimized profits and sustained business growth.

Table of Contents
What is a clinical data strategy?
It is a standardized method employed by healthcare institutions to efficiently manage and leverage their clinical data. This encompasses the systematic collection, storage, and analysis of healthcare data, ultimately enhancing patient care, supporting research endeavors, and aiding decision-making processes. The primary objectives of such strategies are to uphold data integrity, ensure privacy, and fortify security, all in alignment with regulatory mandates. Implementation often involves incorporating electronic health data record systems and using data analytics technologies to streamline data management. For example, successful strategies have demonstrated tangible benefits such as enhanced patient outcomes, cost-effectiveness, and progress in medical research.
Statistics indicate a widespread adoption of these strategies, with around 82% of healthcare organizations having implemented them. Noteworthy outcomes include a substantial reduction in patient wait times, with reported decreases of up to 35%. Comprehensive clinical data strategy implementation has exhibited a significant 40% boost in healthcare provider productivity. Moreover, these strategies have played a pivotal role in mitigating medication errors, showcasing a commendable 25% reduction in hospitals. Healthcare organizations embracing robust strategies also realize substantial cost savings, with an average annual saving of $2.4 million reported.
Importance of creating and implementing a clinical data pipeline strategy:
- Enable real-world evidence-based line of therapy management: This strategy serves as the essential conduit for harnessing real-world evidence (RWE) to enhance the line of therapy management. By seamlessly collecting, integrating, and processing data from various sources such as electronic health records, wearables, and patient-reported outcomes, the strategy ensures a steady flow of accurate and diverse information. This dynamic pipeline facilitates the generation of comprehensive, real-time insights into patient outcomes, treatment efficacy, and adverse events in real-world settings. Clinicians and researchers can make informed decisions, tailor therapies, and adjust interventions based on this robust evidence. Moreover, data pipeline strategies uphold data integrity, security, and compliance, bolstering trust in RWE. Ultimately, a well-structured pipeline strategy empowers healthcare practitioners to optimize their line of therapy management, advancing patient-centric care through evidence-based practices.
Elevate your healthcare journey with Quantzig’s cutting-edge clinical data pipeline strategy – Empowering precision medicine through seamless data integration and advanced analytics. Discover the future of healthcare innovation today! To understand how,
Request a free proposal- Improvement in drug efficacy: Drug development and discovery is a costly, high-risk, and long process that may take approx. 10-15 years with an estimated cost of approx. $ 1-2 billion for each new drug to be approved for new usage. Clinical Research showed that 90% of clinical drug development fails due to poor strategic planning, lack of commercial needs, unmanageable toxicity, lack of efficacy, and poor drugs. A clinical data pipeline strategy facilitates enhanced drug efficacy by seamlessly collating, validating, and analyzing patient data from diverse sources. This approach enables swift identification of treatment responses, adverse reactions, and patient characteristics. Real-time insights derived from the pipeline aid in tailoring therapies, optimizing dosages, and identifying personalized interventions. This iterative feedback loop, supported by robust data management and analysis, accelerates the development of more effective medications, ultimately leading to improved drug outcomes and patient well-being.
- Improved drug marketing effectiveness: In the pharmaceutical technology field, sometimes patients attempt to purchase drugs alone to avoid the consultancy charges, and chemists or retail store owners sell those drugs to them without any prescriptions. That’s why pharma marketers conduct drug marketing campaigns through linkedin to educate their audience about the consequences of prescribed and non-prescribed drugs and increase their sales volumes. A clinical data pipeline strategy significantly amplifies drug marketing effectiveness by orchestrating a seamless flow of pertinent patient insights. This approach transforms raw clinical data into actionable intelligence which enables pharmaceutical companies to tailor their marketing endeavors more precisely. By analyzing patient demographics, treatment outcomes, and adverse events, companies can identify target patient populations, refine messaging, and tailor promotional activities to align with actual patient needs. Moreover, the strategy’s real-time analytics enable swift adaptation to emerging trends and evolving patient preferences. This data-driven approach fosters more personalized interactions between pharmaceutical companies, healthcare providers, and patients. By substantiating marketing claims with real-world evidence, the strategy bolsters credibility and trust and enhances data management.
Key benefits:
- Reduced patient dropout rate
In most healthcare organizations’ environment, the patient dropout rate increases due to a lack of understanding and engagement, scheduling and time conflicts, financial costs, long-distance traveling, and stress. The research strategies play a pivotal role in curbing patient dropout rates by fostering proactive engagement and personalized interventions. By integrating data from electronic health records, wearables, and patient-reported outcomes, healthcare providers gain real-time insights into patient progress and challenges. This enables timely interventions and personalized care adjustments, enhancing patient satisfaction and adherence.
The strategy’s data-driven insights also facilitate targeted communication which allows healthcare teams to address concerns, provide relevant information, and offer support promptly. Predictive analytics from the pipeline help identify patients at risk of dropping out and enable proactive outreach and tailored interventions to mitigate barriers.
- Reduce the cost of therapy
A health data strategy offers a multifaceted approach to diminishing therapy costs through data-driven optimization. By integrating data from various sources like electronic health records, treatment outcomes, and patient demographics, healthcare providers can identify cost-effective interventions and tailor therapies to individual patient profiles. Real-time monitoring and predictive analytics enable early detection of treatment inefficiencies or adverse events, allow timely adjustments, and prevent costly complications.
Furthermore, the strategy enhances resource allocation by providing insights into therapy effectiveness, enabling informed decisions on treatment modalities, medications, and interventions. By leveraging these insights, healthcare organizations can streamline workflows, reduce unnecessary procedures, and minimize trial-and-error approaches, all of which contribute to cost reduction. Overall, the clinical data pipeline strategy empowers healthcare providers to implement evidence-based, cost-efficient therapies that prioritize patient well-being and financial sustainability.
- Improved patient mapping rate across data sources
Though difficult, effective patient journey mapping is an invaluable procedure for health systems. Having an entire picture of how a patient accesses and moves through the health system allows healthcare administrators to understand how an organization is successfully performing at each touch point. For the patients, it leads to better-informed patient outreach efforts, enhanced patient experience, and a higher-quality patient care experience overall. If all essential patient data lived together on a well-crafted unified platform instead of disparate data silos, it could be easy for health systems to better connect all data points to map the entire patient journey, from referrals to scheduling and beyond.
In this case, it serves as a vital tool in enhancing patient mapping rates across disparate data sources asset. By unifying data from electronic health records, claims, wearable devices, and more, the strategy facilitates data management, data monetization, accurate patient identification, and matching. Robust data cleansing, normalization, and integration processes ensure consistency and quality, mitigating errors in mapping. This strategy also leverages advanced algorithms and machine learning techniques to resolve discrepancies and create reliable patient identifiers, reducing duplication and enhancing cross-referencing. Additionally, real-time updates and continuous synchronization between data sources contribute to maintaining accurate patient records.

The use cases:
In the dynamic realm of healthcare, the creation and implementation of a robust strategy have become paramount for healthcare organizations aiming to revolutionize patient outcomes, drive innovation, and optimize treatments. At its foundation, this strategy hinges on meticulous data management, ensuring that data sources are integrated seamlessly, thereby fostering interoperability, security, and governance. As healthcare organizations embark on research endeavors, including clinical trials and drug development goals, the need for a cohesive data architecture becomes imperative, setting standards that align with regulatory compliance.
Technology integration serves as the linchpin for this strategy, weaving together digital infrastructure, analytics tools, and information systems to facilitate data collection, analysis, and reporting. By leveraging advanced analytics approaches and biometrics services, organizations can derive actionable insights, enabling evidence-based decision making and enhancing patient care. Collaborative efforts between teams’ vision, comprising executives, sponsors, experts, and participants, ensure that the clinical trial processes level is streamlined, from planning topics to execution input, addressing the inherent challenges and contribution of complexity, risk management analyses, and efficiency.
Furthermore, as healthcare company navigate the multifaceted landscape of regulations, standardization, and quality management careers, a well-defined data strategy emerges as a cornerstone. Such strategies encompass a variety of initiatives, from data collection and analysis to reporting and compliance, ensuring that therapies and treatments are grounded in evidence-based practices. The integration of clinical trial results, patient data, and biometrics services fosters a holistic view of patient outcomes, enabling organizations in order to tailor therapies and interventions to individual needs and rights.
As technology continues to evolve, so does the scope and impact of a clinical data pipeline strategy. Organizations must remain vigilant, continually updating their platforms, tools, and models to address emerging challenges, risks, and opportunities. The proliferation of webinars, white papers, and content underscores the industry’s commitment to education, best practices, and innovation, ensuring that healthcare professionals remain at the forefront of research demands and development.
In conclusion, the strategic creation and implementation of this strategy encapsulate a harmonious blend of technology, products, leadership, and collaboration. By prioritizing patient outcomes, compliance, and efficiency, healthcare organizations can navigate the intricate landscape of drug development, clinical trials, and treatments. As the industry continues to evolve, the importance of a cohesive data strategy cannot be overstated, setting the stage for innovation capabilities, success, and excellence in patient care.
Conclusion:
In the dynamic landscape of healthcare industry, the creation and implementation of a robust clinical data pipeline strategy stands as a cornerstone for realizing the full potential of data-driven innovation. By seamlessly orchestrating data acquisition steps, validation, integration, and analysis, this strategy empowers healthcare institutions to make informed decisions, drive evidence-based practices, and advance patient care. The strategy’s role in enhancing interoperability, security, and data quality questions cannot be understated, fostering collaboration, trust, and compliance. As healthcare evolves, a well-executed data pipeline strategy serves as a catalyst for transformative outcomes that enable healthcare professionals to optimize therapies, streamline operations, and ultimately improve patient well-being.
Quantzig’s expert team help your organization unlock the true potential of your data. Discover now!
Request a no-cost pilotSuccess Story:
Streamlining Healthcare Insights: How Quantzig Revolutionized Clinical Data Pipeline Strategy Implementation
Client Details: A prominent healthcare institution located in the United States faced challenges in harnessing its vast troves of patient data to drive informed decision-making, streamline operations, and enhance patient outcomes. They sought to implement a robust clinical data pipeline strategy to address data silos, ensure data accuracy, and facilitate data management.
Challenges:
- Low patient map rate across EHR, claims, and drug databases
The client encountered challenges with a low patient mapping rate across electronic health records (EHR), claims, and drug databases. Inaccuracies in patient identification and matching led to fragmented data, hindering comprehensive insights and patient-centric care. Discrepancies in data formats, naming conventions, and data entry errors exacerbated the issue. This fragmented view impeded research accuracy, care coordination, and treatment optimization.
- Siloed planning of drug development based on uni-dimensional patient data
Besides, they grappled with challenges stemming from siloed planning of drug development relying on uni-dimensional patient data. Isolated data from disparate sources hindered holistic patient insights and accurate treatment evaluation. Lack of integration obscured potential interactions, adverse effects, and real-world efficacy. This fragmented approach prolonged development cycles, inflated costs, and risked inadequate patient outcomes.
- Low initial adoption due to poor marketing effectiveness
The client faced challenges related to the poor initial adoption of their product attributed to poor marketing effectiveness. Their messaging failed to resonate with the target audience resulting in limited awareness and engagement. They struggled to communicate the product’s unique value proposition which also led to misconceptions about its benefits. Additionally, inadequate market research hindered their understanding of customer needs and preferences, causing misalignment between the product and its intended users. The absence of a coherent marketing strategy, including digital presence and customer engagement, exacerbated the issue.
Solutions:
- A unified patient registry database that combines drug, EHR, and claims data
The implementation of a unified patient registry database, amalgamating drugs, electronic health records (EHR), and claims data, profoundly benefitted the clients. This integrated repository eliminated data silos and enabled comprehensive patient profiles. The synergy of drug data facilitated insights into treatment outcomes, adverse events, and drug interactions, enhancing drug development and safety monitoring with medical device. EHR integration enriched patient histories, allowing personalized care decisions and request. Claims data integration provided cost and reimbursement insights, optimizing resource allocation. The unified database streamlined research endeavors improved patient matching accuracy, and empowered evidence-based decision-making.
- Setup OMOP schema to report real-world patient data
The establishment of the OMOP (Observational Medical Outcomes Partnership) schema for reporting real-world patient data brought significant advantages to the client. By adhering to this standardized data model, the client gained the ability to transform diverse and complex patient information into a structured format, promoting interoperability and cross-study analysis. This facilitated streamlined data aggregation from various sources such as electronic health records, claims, and clinical trials. The OMOP schema enabled the client to perform robust analytics, uncover hidden insights, and identify trends across different patient populations and therapeutic areas. Furthermore, this approach fostered collaboration with research networks and regulatory bodies, accelerating regulatory submissions and expediting drug development.
- Patient journey database infrastructure
Our team implemented a patient journey database that captured the entire healthcare experience of patients, from initial interactions with healthcare providers to treatment outcomes. By consolidating data from various touch points such as appointments, diagnoses, treatments, and follow-up visits, the client gained holistic insights into patient pathways. This allowed for the identification of bottlenecks, inefficiencies, and focus areas for improvement in care delivery. The database enabled data-driven decision-making among groups, enhancing care coordination, payers’ decisions, personalized treatments approval, and patient satisfaction. Additionally, it facilitated research by providing a comprehensive view of patient cohorts, aiding in the design of clinical trials and real-world evidence studies. Ultimately, the patient journey database empowered the client to optimize patient care, streamline operations, and drive evidence-based healthcare improvements.
Impact Delivered:
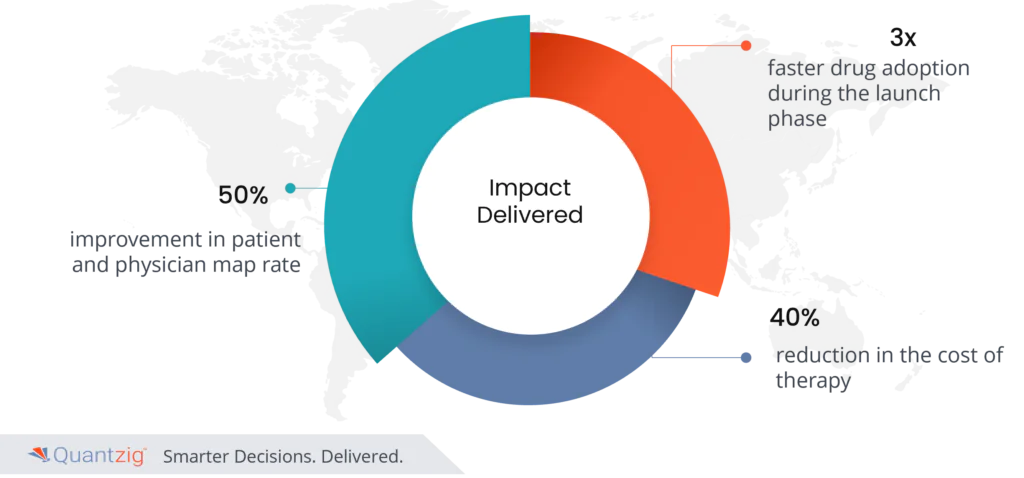
- 50% improvement in patient and physician map rate
- 3x faster drug adoption during the launch phase
- 40% reduction in the cost of therapy
Ready to Transform Your Data Strategy?
Subscribe Quantzig today to discover how our expertise can help your organization unlock the true potential of your data, drive innovation, and gain a competitive edge.


